 |
Rule by the Margate Local Board of Health 1851 - 1858
Anthony Lee
1. The Public Health Act of 1848.
Until the middle years of the nineteenth century the role of government was understood to be the defence of the country and the administration of the law; there was no suggestion that the government should provide money out of taxation for social purposes such as education or health. Education was provided by private schools, for those who could afford it, with some basic schooling for the children of the poor, funded by charitable donations. Health was in the hands of private doctors, who charged for their services, and hospitals funded largely by charitable endowments. But with the ending of the wars with France and the return of prosperity in the late forties and early fifties, thoughts turned to social reform, to the improvement of towns and cities and the removal of the corrupt bodies running many of them, and to a solution to the ‘problem’ of the poor. The Whigs, the precursors of the modern Liberal Party, were then in power and they embarked on a wholesale reorganization of the relationships between central and local government aimed at improving the conditions of the poor.1
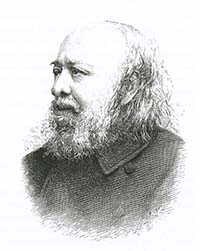 |
Edwin Chadwick |
In 1832 the government established a Royal Commission to report on the workings of the old poor law, with Edwin Chadwick, a committed social reformer, as one of its most active members. Their report resulted in the passing of the Poor Law Amendment Act of 1834 which introduced a national network of workhouses, answerable to a central body, the Poor Law Commission; Chadwick became Secretary of the Commission. He hoped that the new Union Workhouses would provide schooling for the children of the poor, and that the infirmaries attached to the workhouses would provide the poor with at least a modicum of health care. Unfortunately his hopes were only partially fulfilled, his plans being opposed by many of the Poor Law Guardians appointed to oversee the workhouses. To be fair, the Guardians faced a serious dilemma, as improving the conditions of the poor would cost money, and that cost would make them unpopular with the ratepayers who had voted them into position. Undeterred, Chadwick continued to fight for improved social conditions, particularly for improved sanitation which he thought would have a major impact on the lives of the poor. Helping to make his case, a series of epidemics swept through the country at about this time, two influenza epidemics between 1831 and 1833, a cholera epidemic in 1831, scarlet fever in 1834, and further waves of influenza, smallpox, typhus and typhoid, before cholera returned in 1848.2
In the Fourth Annual Report of the Poor Law Commissioners published in 1838 Chadwick argued that sanitary reform would actually save money in the long term: ‘all epidemics and all infectious diseases are attended with charges, immediate and ultimate, on the poor rates’.3 Probably as a result of Chadwick’s arguments, Charles Blomfield, Bishop of London, moved in the House of Lords for an inquiry into the sanitary conditions of the labouring classes.4 This resulted in Chadwick’s monumental Report on the Sanitary Condition of the Labouring Population of Great Britain published in 1842.5 The report was clear and hard hitting and led to the passing of the Public Health Act in 1848.6 The act established a General Board of Health, based in London, overseeing a number of local Boards of Health; the General Board had three members, one of whom was Chadwick. Chadwick had no faith in the ability of the existing forms of local government to deliver the changes he thought necessary, and so he ensured that the Act gave the General Board the power to act over the heads of local government when necessary.
The Act described two ways in which a local Board of Health could be established. First, the General Board could impose a local Board of Health on any town where the annual death rate was higher than 23 per 1,000 inhabitants (the average death rate at the time was 21 per 1,000).1 The second procedure for triggering the Act was truly innovative; if more than ten percent of the rate payers of a town petitioned the General Board of Health asking for the Act to be applied to their town, the Board would send an inspector to the town to conduct a public enquiry into its sanitary condition. The inspector would then prepare a report for the General Board and advise whether or not the Act should be enforced. The importance of this clause was clear; ‘All the Act required was that a minority of ten per cent of the ratepayers should petition the Board on one single occasion; all subsequent developments rested entirely with the Board . . . Nine-tenths of the local ratepayers might be opposed to the Act; nay, if the original petitioners should have changed their minds – all the ratepayers might be opposed to the Act, but, provided that, at one time or another a petition had been made in due form, the Board was at complete liberty to apply the Act’.7
The procedure for establishing a Local Board, once it had been agreed that there should be one, was to use a Provisional Order, a procedure designed to keep down costs. The Provisional Order would be issued by the Local Government Act Office, a branch of the Home Office, and would describe how the provisions of the Public Health Act would apply to a particular town. The order would have no effect until it was confirmed by an act of parliament, which is why it was called a ‘Provisional Order’. Discussion between the General Board and the local ratepayers gave an opportunity to introduce any special provisions into the Provisional Order thought to be necessary. The draft Provisional Order would be published and sent to parliament, where it would lay on the table for a month or so, allowing time for discussion of any contentious issues. Final confirmation of the Provisional Order would be by ‘An Act for confirming certain Provisional Orders of the General Board of Health’, each act covering a number of places; for example, the Act 14 and 15 Vict., c. 98, passed on 7 August 1851 covered 18 towns, including Margate.8 The average cost of applying the Public Health Act to a town was estimated to be about £120, compared to an average cost of about £2,000 for one of the old Private Acts.8
The duties of the General Board Inspectors were spelt out in detail in the Public Health Act. At a public enquiry held in the town, they were to examine witnesses, as to: ‘The sewerage, drainage, and supply of water; the state of the burial grounds; and the number and sanitary condition of the inhabitants’.6 The Inspector also had to consider any relevant local Acts in operation in the town and how the ‘natural drainage areas’ mapped onto the existing municipal and parochial boundaries; any mismatch might require a change in these boundaries.